When you think of patient care, you generally don't think of peppermint and lavender. Could peppermint and lavender really make a difference, for example, in easing patient stress? It's something Liezl Moscaya looked into as part of her practicum quality improvement project for her master's degree in nursing.
Trained in the Philippines as a nurse, Moscaya came to the United States, and in 2008, she joined Veterans Administration Healthcare in her home state of Connecticut. Four years later, she decided to do something outside of her comfort zone – start her master's journey at Grand Canyon University.

“I was pretty much scared because all my classmates were very young, and my last academics were pencil and paper, blackboard and eraser,” she said. “Going online with a computer was very scary for me. I thought, ‘How am I going to actually catch up with all these young kids who are in the class?’”
Moscaya started her career as an operating room nurse before moving into nephrology, caring for patients with kidney diseases, then returned to her surgical roots the same year her son left for college.
“I’m doing ambulatory procedures,” she said. “I’m seeing patients before they go into surgery and after they come back from surgery, and I send them home.”
She would see how anxious patients would get before surgery, which would be the beginning of what would become her master's project.
Her report, “Reducing Preoperative Anxiety Using Nonpharmacological Approaches in Veterans: A Quality Improvement Initiative,” originated in her GCU practicum quality improvement project.
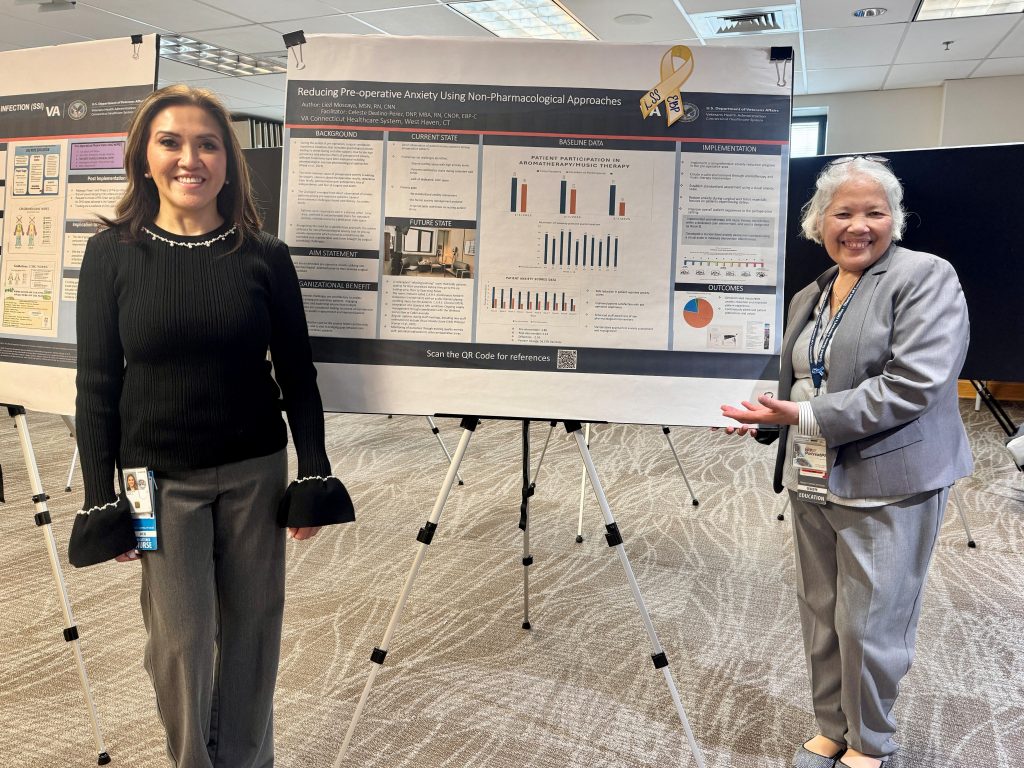
Moscaya, whose master's includes a specialization in health care quality and patient safety, compiled data and observations demonstrating how reducing patient anxiety presurgery resulted in better patient outcomes. Just after earning her master's she was tapped to make a poster presentation of her results at the Veterans Administration Connecticut Evidence-Based Practice Research Symposium.
In November, she'll present her findings at the Nursing Research and Evidence-Based Practice Symposium in Burlington, Vermont, and she'll make a second poster presentation at the Connecticut Nursing Research Alliance Conference later this fall.

Typically, patients with high anxiety are prescribed medication to relax or reduce the fears associated with a surgical procedure. The treatments suppress the symptoms but do not heal the patient.
Moscaya observed in her work and that of other nurses that calming techniques worked better without using meds.
“I researched this because I want to prove it’s right,” she said. “It’s a project initiative, an improvement of basically what we have right now.”
The standard procedure in the VA is different from civilian hospitals, Moscaya said. She shared how there’s everything nurses need, but not a lot of room for patients.
“Waiting time is really bad, sometimes, like hours,” she said. “They’re not sitting, not lying down in a bed. They are lying on a stretcher or sitting in a regular chair in the waiting room.”
The situation ends up amplifying anxiety, according to the research.
“So imagine that you're having a surgery and you're sitting for hours. You don't even want to watch TV, right? Because you're going for surgery. You're not going to watch CNN and listen to the world's problems,” Moscaya said. “So I see this a lot. And I said to myself, ‘If I'm going to do a quality improvement, I'm going to have to start where I actually work, the presurgical unit.’”
Combining stress-reduction techniques, aromatherapy, music therapy and conversation, Moscaya and others in her department started separating patients into common groups. Some wanted music, some quiet and others liked the aromatherapy.
“I mixed peppermint and lavender, and it really works,” she said. “Sometimes the patients fall asleep and we have to wake them for surgery.”
She would ask patients about their anxiety level before starting the nonpharmacological treatment. She asked who wanted music and who wanted aromatherapy. Then after the improved process, she’d ask them about their anxiety levels.

“I compared the results,” she said. “The actual outcome was really amazing. How can you say ‘no’ to being calm?”
Some people wanted to watch the news, so she set up another room for them. In the end, she found out that she was not alone in her discovery.
“So, I researched and found that a lot of the hospitals are doing it too,” Moscaya said. “That's when evidence-based actually entered. It's not just the hospital where I work. Other hospitals are offering (this approach). The data between the other hospitals (and the VA) are amazing.”
Between the demands of her career, her work on her master's, and her passion for her patients, faith kept her on the path.
“I'm very lucky to be at Grand Canyon (University) because of it being Christian faith-based,” Moscaya said. “A discussion board we have uses the Christian principles that we apply. I actually was thankful to be guided through, even though I'm Catholic.”
The 30-minute commute to work every day is her time to pray.
“That's all I have. I have 30 minutes,” she said. “I don't play any music; I don’t talk on the phone. The 30 minutes before going to work is my prayer time.”
It’s all part of her commitment to her patients. The prayer time and her faith on the job guide her.
“I feel, as a nurse, I'm spiritually responsible to my patients,” Moscaya said. “And I've been very lucky that this profession, through my faith, is giving me an opportunity to be an instrument of healing and comfort.”
GCU senior writer Eric Jay Toll can be reached at [email protected].
Related content:
GCU News: Faith, fatherhood and the front lines: A veterans road to healing through nursing
GCU News: Her nursing journey encompasses 3,000 miles, 16 months, 3 states and her faith








































